The pandemic has dealt the final blow to him, but the traditional model of communication with health professionals (HCP) had already been in crisis for some time. Progressively stricter regulations and the advent of digitalization had sprung the weapons of the scientific informant and made meetings at offices and clinics less and less effective.
With the restrictions on travel and social contacts due to the pandemic – especially in healthcare environments – the process has undergone a decisive acceleration, changing – perhaps forever – the reference scenario. Despite their success, however, digital tools still leave various information needs unmet.
Digital Tsunami
Already in 2016, a survey among HCPs from various specialist areas revealed that over 70% of doctors use Dr. Google for professional purposes on a daily basis: oncologists, in particular, search for information on the web at least four times a day. A CMI / Compass survey two years later revealed that four out of five doctors are searched via smartphones.
The Covid-19 pandemic has given a sudden impetus to the digitization process by transforming IT enabling from an optional option to a necessity and forcing many realities – not only in the pharma sector – to suddenly convert to completely virtual models.
A Deloitte report dedicated to life sciences reveals that in April 2020 – the first in complete lockdown – companies sent seven million emails (almost six times higher than in January) and conducted 317,000 meetings from remote (about 65 times the number of videocalls at the beginning of the year). The transition to the virtual world, however, did not solve the problems of updating the HCPs.
Unmet information need
Although traditional in-person visits have abruptly stopped, the need for updated information remains intact, not least because the data load in the healthcare sector doubles every twenty years.
According to research published this year, nearly 90% of doctors search for information on medicinal products several times a day (49%) or several times a week (39%).
An article in Jama reveals that despite the wealth of content available, doctors in most cases still rely on memory (which, according to another study, is quite fallacious, due to outdated knowledge or incorrect information). Online channels do not prove sufficient to fill the gap: a meta-analysis published at the beginning of 2022 verified that the percentage of questions that are answered by the web varies from 23% to 93%.
One of the problems is undoubtedly the lack of time available to doctors to carry out research. It has been calculated that during a visit to a patient, a professional only has two minutes to find an answer while after the session is over he spends more than half an hour. However, these results are limited to the time it takes to retrieve a single item.
Sources also vary according to the time available: according to a survey published in Pharmaceutical Medicine, healthcare professionals preferably use digital media when information needs to be found quickly (within 10 minutes), but when they have more time (1-2 days). ) prefer to rely on more traditional resources such as printed magazines, institutional health websites, but also informants from companies.
The amount of information available and the immediacy of access are the strengths of digital technologies but also their Achilles’ heel. In 1964, the American social scientist coined the term Information overload to indicate a situation in which the excess of information inhibits the decision-making abilities of an individual.
This mechanism also occurs with health professionals struggling with the uninterrupted flow of the web. A study published in the International Journal of Medical Informatics explains that the most critical aspects for doctors who use the Internet are the excess of information, the lack of adequate skills to carry out research on the net, and a lack of knowledge of available sources.
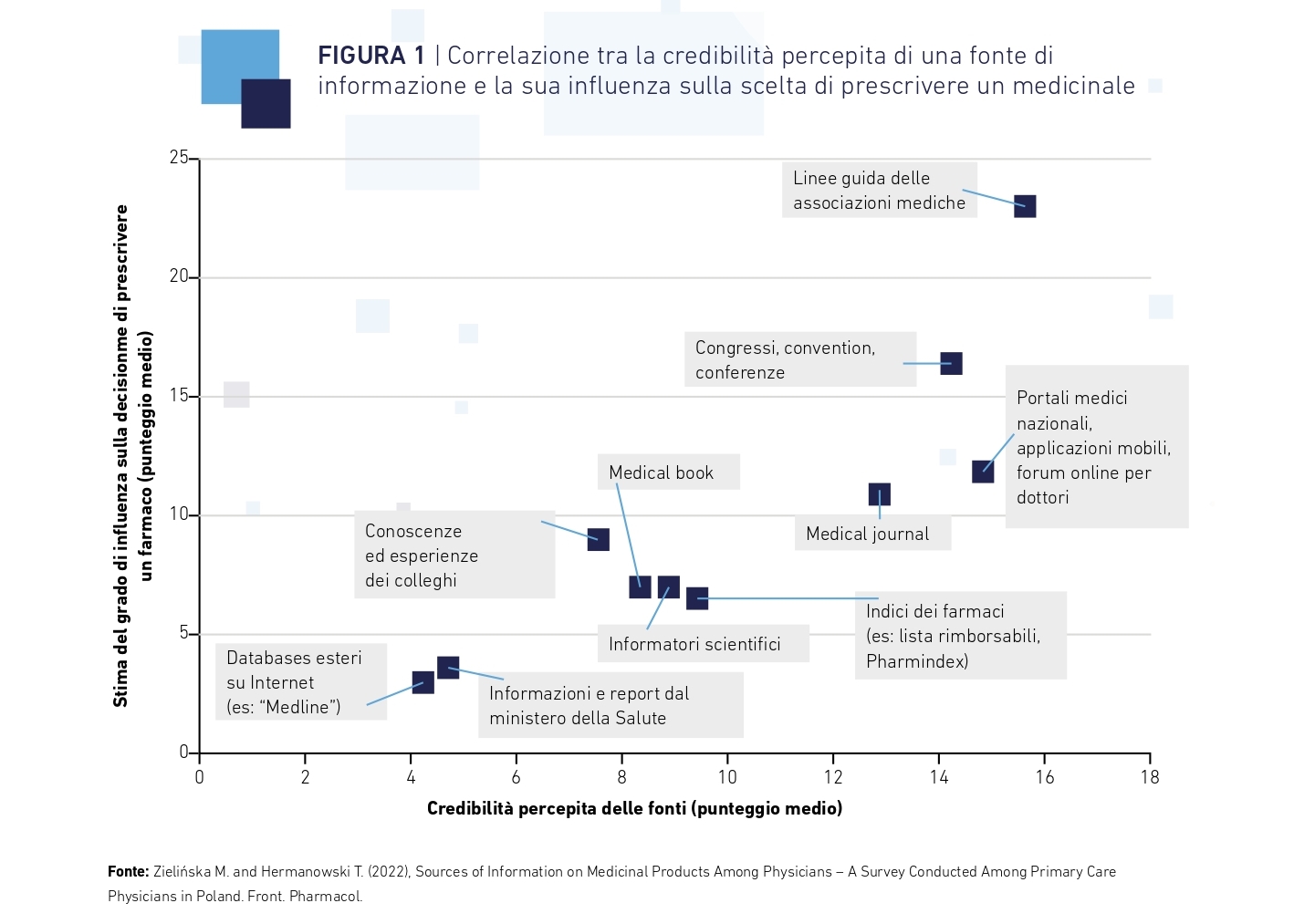
A survey carried out by the University of Warsaw also found other critical issues, such as a lack of knowledge of foreign languages and the inability to assess the credibility, statistical significance and clinical value of the information collected. For this reason, doctors prefer to rely on reliable sources such as the guidelines of medical associations, congresses (even virtual ones), medical journals and books and even the advice of colleagues.
Not just digital
The unstoppable drive towards digitalization, however, did not put out the face-to-face relationships. In a survey carried out on LinkedIn among pharmaceutical industry representatives, 72% of respondents say they are convinced that the use of digital platforms and social media will increase in the future but believe that even in-person meetings, congress activities and events education will continue to play an important role.
Communication through social media, in fact, is considered less effective – if not mediocre – by 90% of respondents, while the same percentage considers face-to-face interaction the most effective communication channel.
Other forms of face-to-face interaction, such as panel discussions and hospital meetings, are also seen as effective as are promotional activities at conferences.
The survey highlights the continuing need for face-to-face interactions, but clearly highlights how these need to be conducted in a more scientific and, very often, non-promotional environment, in line with transparency guidelines.
The objectives of the personal meeting must change. The Deloitte report underlines how the meetings must be designed as an initial step of an engagement process that will take place above all virtually.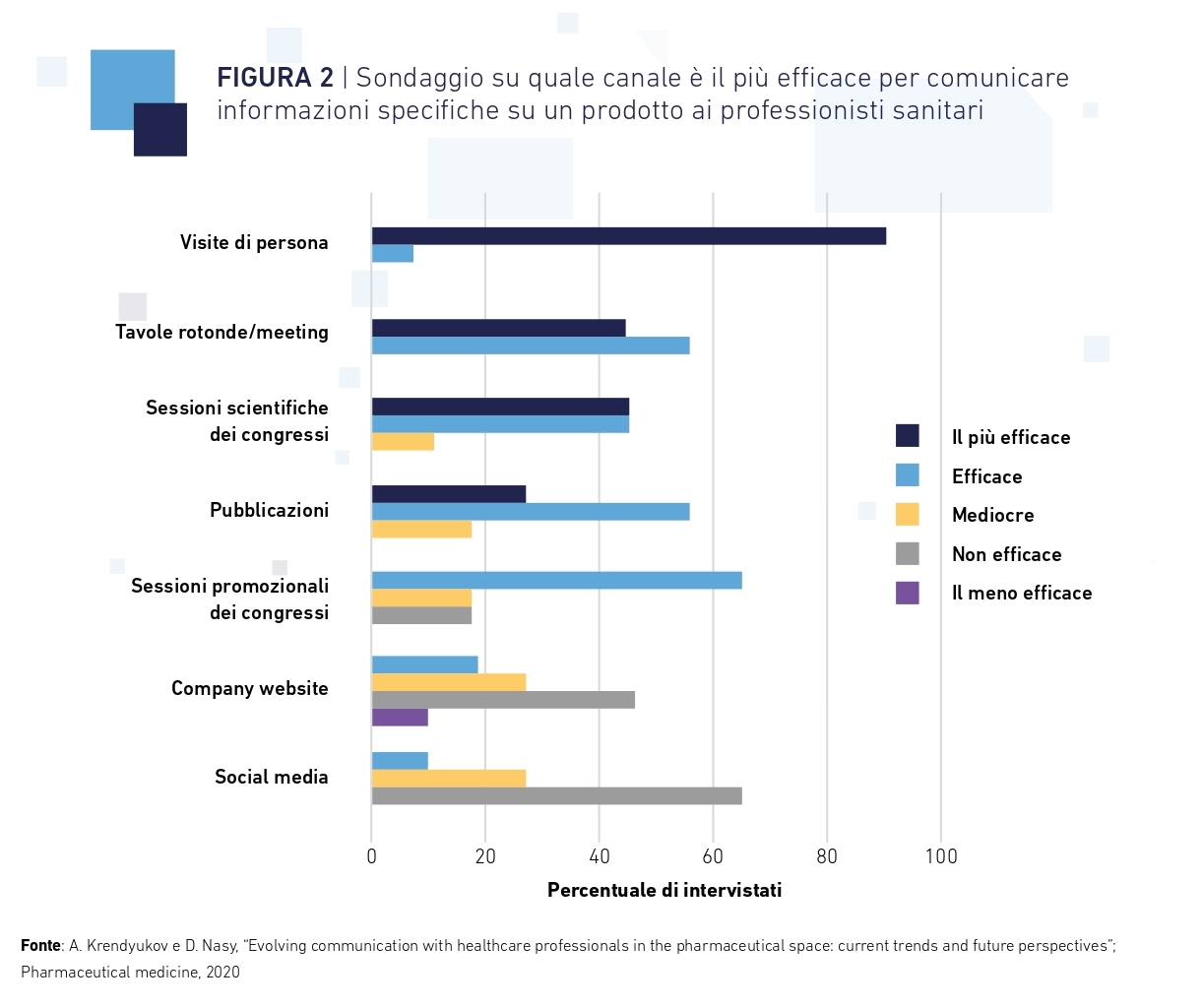
The role of the medical affair
In this, it will be essential that company representatives develop empathy and the ability to understand the needs of individual professionals. “The new relationships – explains the report – can be deepened by contents in tune with the individual needs of HCPs and by actions that demonstrate understanding and empathy”.
Paradoxically, the pandemic may have improved the relationship between companies and doctors even during virtual visits. According to the Deloitte report, “during the pandemic, some pharmaceutical representatives reported having 30-minute conversations with healthcare professionals, up from five in previous periods.”
In this context, representatives of companies able to understand scientific topics, interested in patients and able to sustain meaningful discussions with HCPs will take decisive action.
A particular role will be played by assistance on medtech products, which are closely related to device maintenance and technical support. Experts believe that the best candidates to lead this transition are Medical Affairs, which are destined to assume an increasingly significant role at both the strategic and operational levels. With in-depth knowledge of the product, disease and regulations, the Medical Affair and Medical Science Liaison teams have the right tools to communicate effectively with health professionals.
From push to pull
In any case, communication can no longer be guided by the promotion of a product. The pharmaceutical sector must become a reliable guide of the scientific world for the therapeutic areas of expertise, providing high quality content regardless of brand association. Communication must transform from “push” to “pull”.
Rather than structuring a one-sided flow of information to the health professional (push), companies must create – or exploit – environments in which HCPs converse – perhaps with patients – by discussing mechanisms of action, scientific principles, problems, and revealing their real needs.
It will be up to the company to enter this flow to respond appropriately (pull) to emerging needs. In this way they will be able to convey to the interlocutors a sense of collaboration and partnership.
Given that three out of four HCPs more easily consider content if it comes from a reliable and known source, it can be useful to involve opinion leaders linked to known realities. “The use of reliable third-party content – says Alessandro Gini, one of the first in Italy to become a LinkedIn expert and trainer – allows you to validate your business, your know-how and confirm the positioning of the company”.
Research confirms this thesis by noting that “over 80% of healthcare professionals are more likely to prescribe a new drug if it is approved by a clinical expert”.
#Events
The best way to fit into the flow of information to professionals is to be where they are, even online.
Congresses, conventions and conferences represent one of the most reliable updating channels and the digital component increases the possibilities of interaction of these events. During the 2018 annual meeting of the American Society of Clinical Oncology (Asco), the official hashtag of the event generated over 90,000 tweets in five days with over 20,000 unique authors and 500 million potential impressions.
From social media to AI
In addition to information on diagnoses and treatments, doctors need help in dealing with patients in the virtual world.
Key requests include digital patient education tools, remote care guidance, and information to help patients access labs, testing and imaging.
There are many tools available to help HCPs: animations, videos, interactive online courses, webinars, newsletters, podcasts, etc. Artificial intelligence also has enormous potential: chatbots and virtual assistants are already a reality.
Tabatha, for example, is a Facebook bot made by Boehringer Ingelheim and aimed at asthma patients. Or there is Virti, a virtual patient designed to develop the soft skills of healthcare professionals: doctors learn how to communicate diagnoses and treatment plans in difficult situations, and to build a relationship of trust with the patient.
A study found that the virtual and augmented reality approach increases memorization by 230% compared to standard training.